The use of technology in the healthcare industry has led to AI-enabled diagnostics, digital therapeutics, virtual health assistants, personalized care, and much more. While this has transformed patient care delivery, it has simultaneously exposed electronic Protected Health Information (ePHI) to significant risks and vulnerabilities.
USA federal records show around 385 million breaches of patient records from 2010-2022. According to these records, there are 792 active healthcare data breach cases under investigation in the last 24 months. From heavy penalties to operational disruptions, the consequences of improper management of ePHI can be severe. Thus, laws like HIPAA are required to govern healthcare service providers for the management of ePHI.
As the digitization of healthcare is rightly celebrated, it is also critical to know why ePHI security is central to this motive, the risks it carries if overlooked, and what all organizations can do to fortify themselves in such cases.
Inside ePHI: What is Modern Digital Health Data
ePHI or electronic Protected Health Information consists of individuals’ health-related data in electronic form. It includes the electronic information that can be used to identify a patient along with data regarding diagnoses, treatment plans, insurance details, and medical history.
While ePHI is a subset of PHI. ePHI exists only in digital form, while PHI can include paper records, verbal communications, or physical documents.
Since HIPAA governs PHI, the same applies to ePHI only if it qualifies under the following conditions:
- It should contain information on a patient’s medical history along with present health condition, provision of healthcare services, and payment.
- It should contain at least one of the 18 HIPAA personal identifiers, like name, telephone number, geographic information, SSN, biometric identifiers, etc.
How HIPAA Regulations Secure Electronic Health Data?
All covered entities, like healthcare organizations and related business associates, must comply with the HIPAA Privacy Rule & Security Rule in order to achieve HIPAA compliance. The Privacy Rule defines how all forms of protected health information should be used and limits its disclosure. Meanwhile, the Security Rule concerns itself specifically with the protection of ePHI.
HIPAA Security Rule requires covered entities to follow administrative, physical, and technical safeguards in order to ensure ePHI is accessed only by authorized personnel and remains protected from unauthorized access. These safeguards include enforcing authorized access, training staff, and performing periodic audits. Additionally, when retiring old assets storing ePHI, they must be securely wiped to ensure proper data disposal.
These safeguards help healthcare organizations not only protect sensitive patient data but also help in achieving HIPAA compliance.
Neglecting ePHI Security: A Threat to Patient Trust and Compliance
ePHI security is often overlooked and is usually neglected by organizations due to varying reasons like budget constraints, underestimation of related threats, and so on. While it is treated mainly as a compliance checkbox, neglecting ePHI security can gravely cripple an organization as well as endanger patient privacy.
Let’s take a look at the most critical risks that can emerge as a result of the negligence of ePHI security:
- Cyber Threats and Unauthorized Access: ePHI contains a lot of sensitive data, including medical history, social security number, & financial details. This information can be exploited if the storage systems are unprotected, not encrypted, and outdated software is used. The data becomes vulnerable to cyber threats and leads to a data breach. Change Healthcare, data breach is one such example. This division of UnitedHealth Group experienced a ransomware cyberattack in February 2024. This affected the personal information of 190 million individuals and disrupted the organization’s operations for several weeks.
- Legal Penalties: Organizations failing to comply with HIPAA rules can be imposed with a penalty of up to $50,000 per violation. The maximum civil penalty that can be imposed for violations goes up to $1.5 million. Whereas, the criminal penalty on individuals can go up to $250,000 or 10 years imprisonment. This leads to financial burden on the organization, alongside reputational damage and loss of customer trust.
- Loss of Patient Trust: Patients place a lot of trust when sharing their personal information with healthcare providers and organizations. This trust is the backbone of the healthcare industry, and loss of the same may lead to the refusal of sharing information by patients, avoidance of digital tools for healthcare like web portals, wearables, etc., and overall reduction of participation in preventive and personalized care for individuals.
- Operational Disruption: If ePHI is exposed and compromised, organizations are forced to shut down and suspend digital operations. This can cause complete operational disruption, leading to delays in diagnosis and treatments, reduced and diverted care, increased clinical risk, revenue cycle disruption, etc.
- Compromised Data Integrity: Failure to protect ePHI not only results in data theft but can also lead to data tampering. This can compromise the integrity of sensitive medical data, bringing about incorrect medical decisions, which can sometimes be fatal, inaccurate insurance claims, and a threat to patient safety.
Since ePHI fuels almost every aspect of healthcare, organizations need to carefully assess such risks and implement robust strategies to tackle them.
Essentials to Manage & Protect ePHI
Securely managing ePHI is extremely important for organizations. This is required for maintaining data integrity, security, and above all, compliance with laws and regulations. It is therefore critical for organizations to develop strategies that assist in implementing controls across all systems and processes.
Given below are a few strategic essentials that organizations can adopt for ePHI protection and management:
- Risk Assessment: Organizations can prevent potential risks by proactively assessing and identifying them before incurring any damage. Risk assessments should be carried out across all hardware, software, and networks in order to identify vulnerabilities in systems, storing, and dealing with ePHI. This will help in the detection of weak points, evaluation of current safeguards, and fostering of critical security efforts.
- Strengthen Access Controls: Limited access to ePHI should be maintained on a need-to-know basis and should be strictly monitored. Multi-factor authentication, session timeouts, inactive account removals, etc., should be implemented to further strengthen access to ePHI. This ensures that only authorized individuals have access, reducing the attack surface and insider threats.
- End-to-end Encryption: End-to-end ePHI encryption should be done across all devices, cloud platforms, backups, etc., using industry-standard encryption for stored data, and the SSL protocol should be followed to secure ePHI when it is in transit. Encryption will make the data unreadable even if it is intercepted or stolen, making it an effective security measure.
- Employee Training and Awareness: Digital discrepancies may at times contribute to data breaches, but human error is still a leading cause for major data breaches. Organizations need to conduct training sessions for employees on cyberattacks, secure data handling, and HIPAA compliance. This will help them to understand the importance of secure data handling, especially when it comes to ePHI.
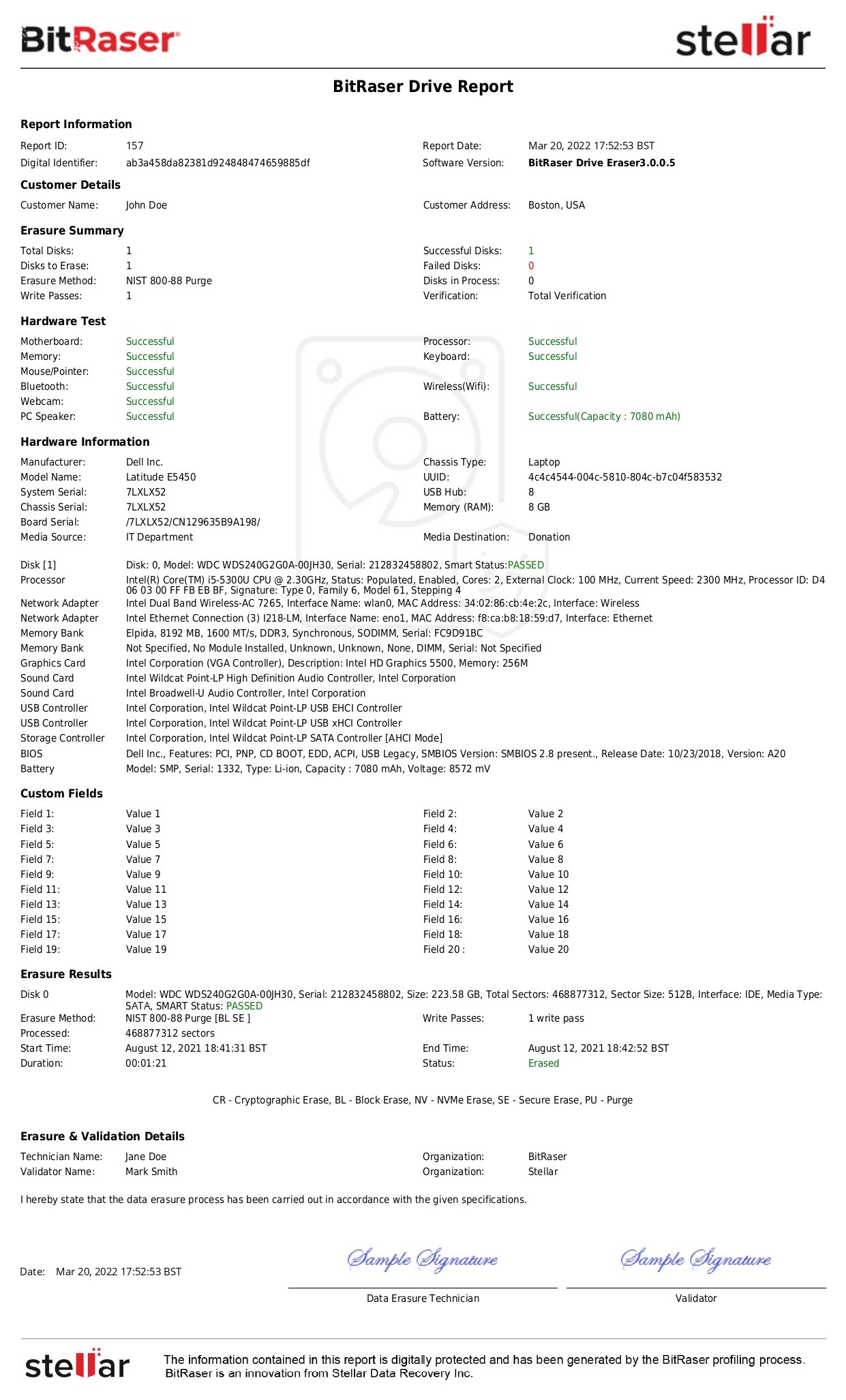
- Secure Erasure and Data Disposal: HIPAA clearly outlines the various retention periods for different covered entities and business associates. Once over, this data must be securely erased or disposed of after serving its purpose. ePHI data must be securely erased using certified tools. Solutions like BitRaser, compliant with NIST SP 800-88 and DoD 5220.22-M standards, ensure permanent data sanitization with auditable reporting.
- Incident Response Plans and Action Plans: Every organization should develop and test an incident response plan in case a cyber-attack occurs. The plan should consist of containment procedures, handling steps, and recovery protocols. Having an incident response plan allows organizations to take timely action against unexpected and sudden cyberattacks and ensures minimum damage.
Conclusion
ePHI has played a vital role in the digital transformation of the healthcare industry. It has enhanced patient care, operational efficiency, and facilitated medical research and public health. While its benefits are aplenty, it also exposes personal medical information of patients to greater risks, threatening data privacy and security. Therefore, ePHI must be securely managed to keep up with this new digital era in healthcare.